How we work with ACC
Private and public healthcare
New Zealand has a public healthcare system that treats acute health conditions and provides some elective surgery. We also have a public, no-fault accident insurance scheme Accident Compensation Corporation (ACC) covering accidental injury.
These are effective in providing healthcare support for accidents and acute and urgent care. But public hospitals cannot do everything for everyone.
Private health insurance complements these public services by making private healthcare available.
How we work with ACC – the Southern Cross member advocacy team
Southern Cross Health Insurance (Southern Cross) cares about the health and wellbeing of our members. In an effort to support you when you undertake an ACC review, the Southern Cross member advocacy team is there to help.
One of the ways Southern Cross helps is by offering all our members an advocacy service to review an ACC decline from either a personal injury caused by an accident, treatment injury or a work-related gradual process. There is no charge for this service for our members.
If the medical evidence shows that your ACC decline may be incorrect, and your treating specialist is willing to provide a supportive opinion, the Southern Cross member advocacy team may be able to assist. We can guide you through the process of an ACC review, providing knowledge of the system and support with the goal of having the ACC decline overturned and the treatment funded by ACC. If successful, you may be able to request backdated compensation and other entitlements from ACC.
We generally assist members who have recently received an ACC decision declining funding for surgery, or a decline of cover for a physical injury related to this. If you have received an ACC decision about something else, we may not be able to assist.
John's story
Southern Cross member John is grateful for the help he received with his declined ACC claim from the Southern Cross member advocacy team. To see how the member advocacy team can help you, watch John's story here.
Who covers what?
ACC has three categories of cover: personal injuries caused by an accident, work related gradual process injuries, and treatment injury. The different categories of cover are treated differently by ACC and therefore by Southern Cross.
Southern Cross policies do not cover treatment for injuries which ACC has agreed to cover. If your treatment relates to an injury or health condition which is covered by ACC, you or your doctor must, therefore, apply to ACC for treatment funding in the first instance.
In circumstances where ACC does not pay the full amount charged for treatment you may be able to claim the remainder under your Southern Cross policy. These may include ACC surcharges and partial payments.
Are you covered?
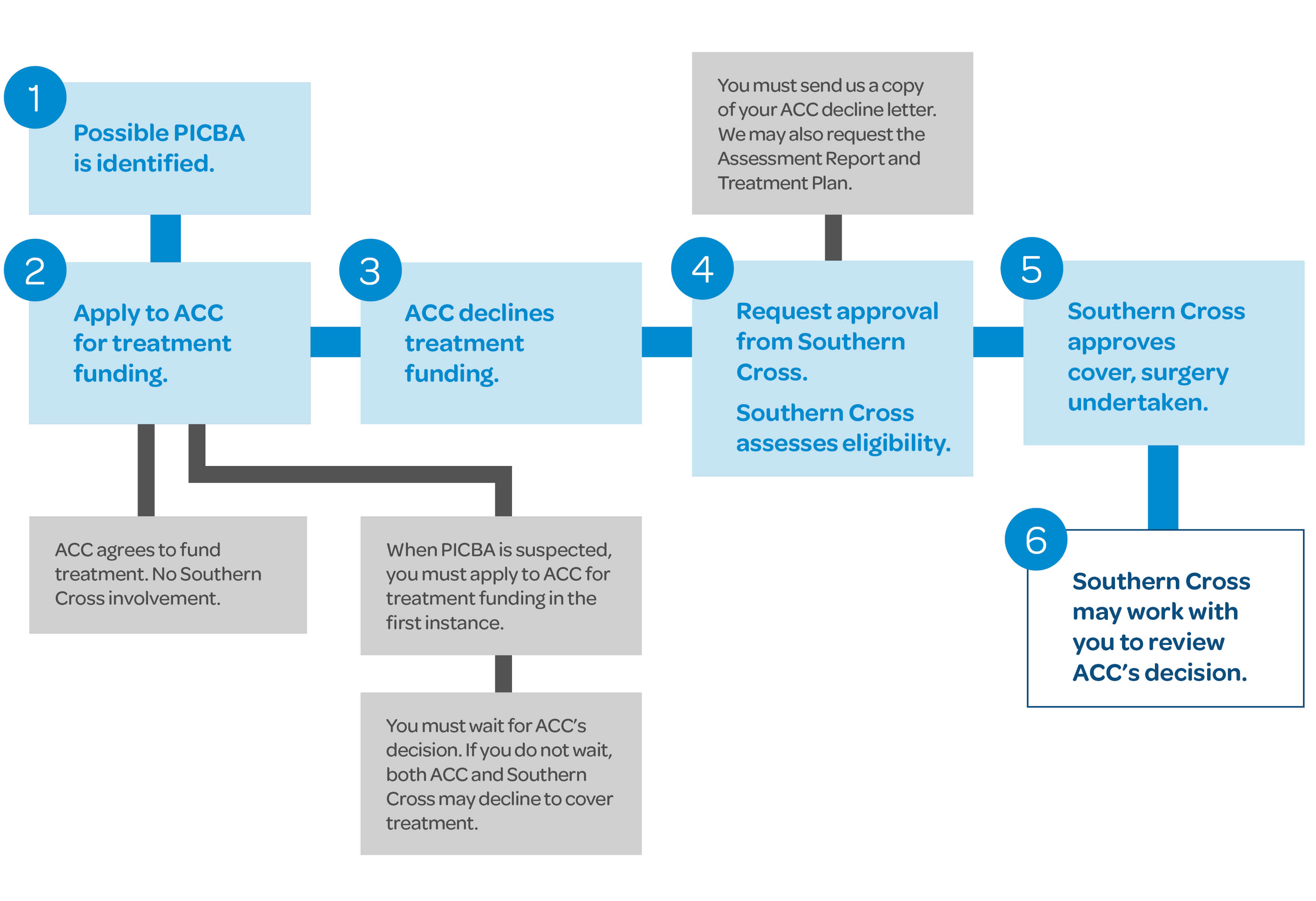
If ACC declines to cover a treatment for personal injury caused by an accident (PICBA)
If your claim is declined by ACC and the treatment you require is covered under your Southern Cross policy, Southern Cross may agree to cover the cost of that treatment. The Southern Cross member advocacy team may also work with you to apply for a review of ACC’s decision. A review can take place either before or after treatment is provided and will not delay your access to treatment.
If you or your doctor think that ACC’s decision is incorrect, and your treating specialist is supportive of your case, please contact the Southern Cross member advocacy Team. We will review the decline documentation and offer advice as to whether a review of ACC’s decision is worthwhile. If there is a case for review of the decision, the Southern Cross member advocacy team can work with you to guide you through the review process.
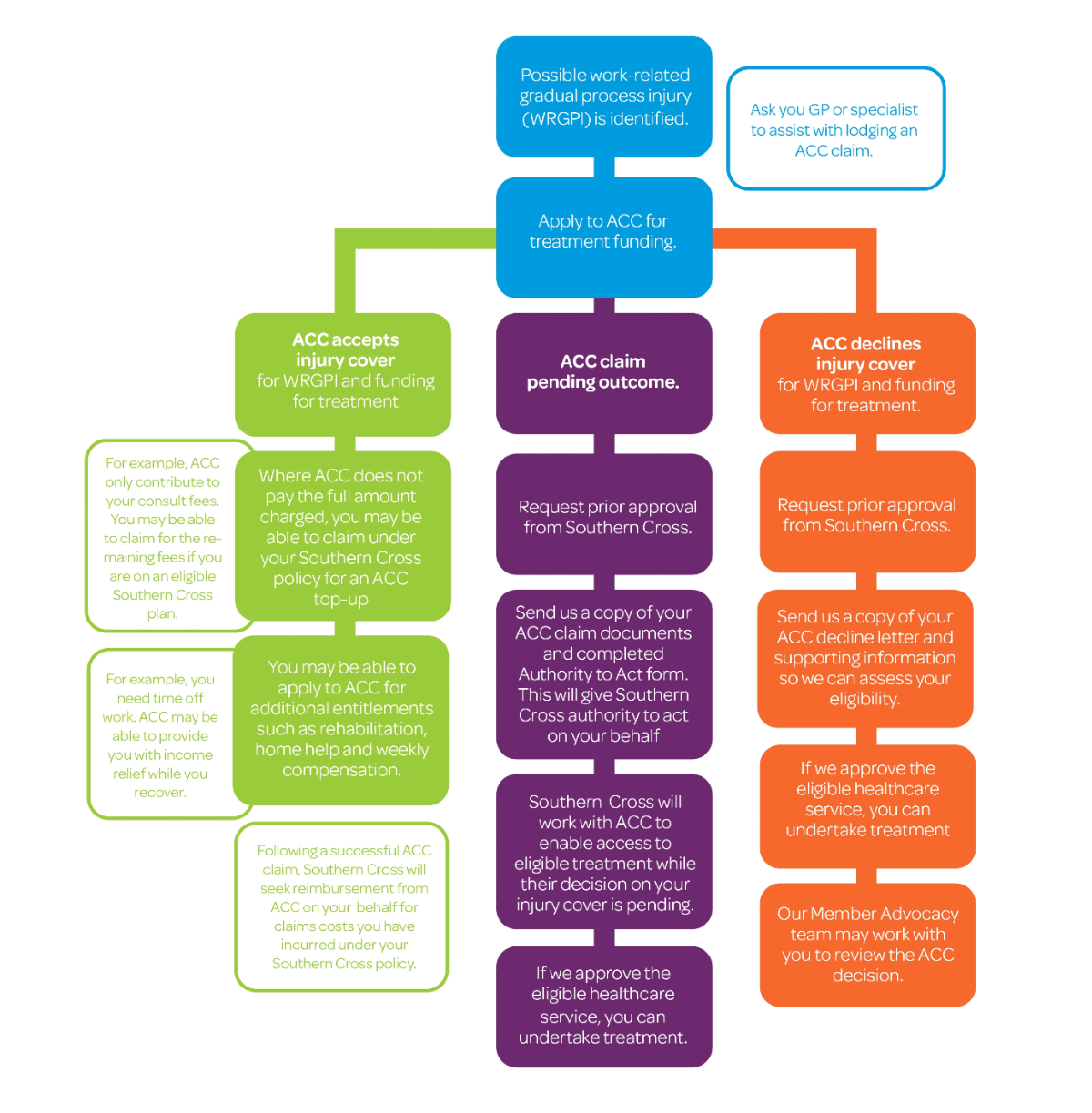
If ACC declines to cover work-related gradual process injury (WRGPI)
WRGPIs are health conditions that develop over time due to the cumulative effects of work-related tasks or environments. These injuries often result from repetitive movements, sustained postures, overexertion, or prolonged exposure to hazardous conditions.
If you believe you may be suffering from a WRGPI, please speak with your GP or specialist about lodging an ACC claim. These types of injuries can be complex, and ACC’s consideration process may take time. If you are a Southern Cross member and require urgent treatment while your claim is being assessed, contact us as we can work with ACC to help you access the care you need while their decision is pending.
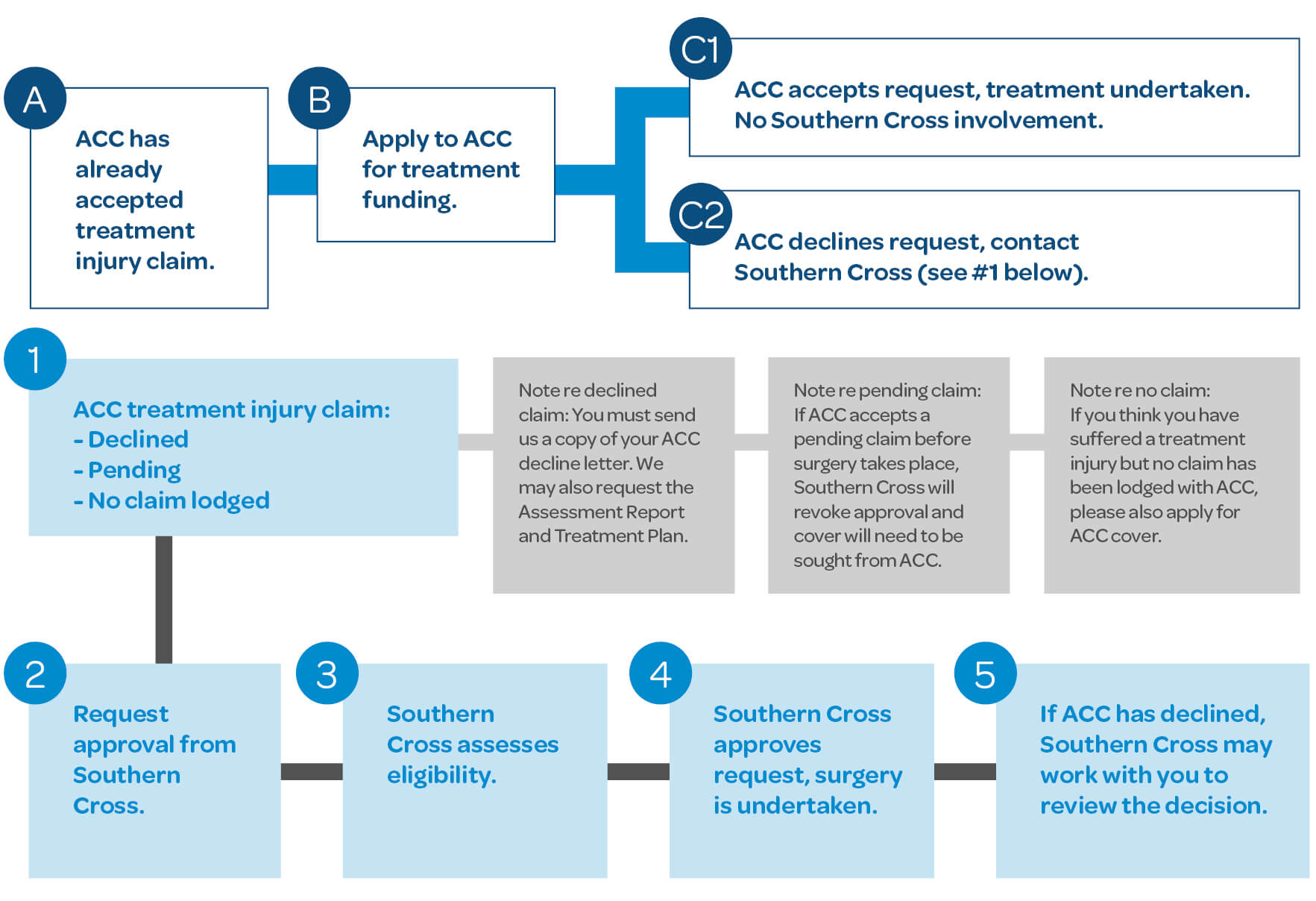
If ACC declines to cover a treatment injury (TI)
Occasionally, a patient suffers an unexpected injury during medical treatment or surgery. If a registered health professional was treating you and the treatment directly caused your injury and is not a normal side effect of your treatment, you may be eligible for ACC cover for a TI.
Unlike a PICBA, ACC does not require a claim to be lodged or a decision on cover or treatment funding to be made before you can undergo treatment for your treatment injury. This reflects the fact that treatment injuries often need urgent treatment and it would not always be possible or appropriate to lodge a claim or request for prior approval before treatment. However, if ACC has already accepted cover for your treatment injury, approval for treatment funding must then be sought from ACC before treatment can take place.
Treatment injuries can be complex, and it is often difficult to determine whether a particular injury meets ACC’s criteria for cover. If you have any questions about whether you may have a treatment injury, you can contact the please contact the Southern Cross member advocacy team for advice.
You may be eligible for ACC entitlements
If your ACC decline is overturned, you may be eligible for ACC entitlements that may include:
- weekly compensation
- rehabilitation (eg physiotherapy, occupational therapy, nurse)
- transport costs (eg treatment, rehabilitation or getting to and from work)
- mobility equipment (eg crutch hire, wheelchair hire)
- home help
- childcare
- other (eg Return to Work programme, Pain Management programme).
Contact the member advocacy team
If you have any questions about this process, please contact the Southern Cross member advocacy team a [email protected] or on 0800 800 181